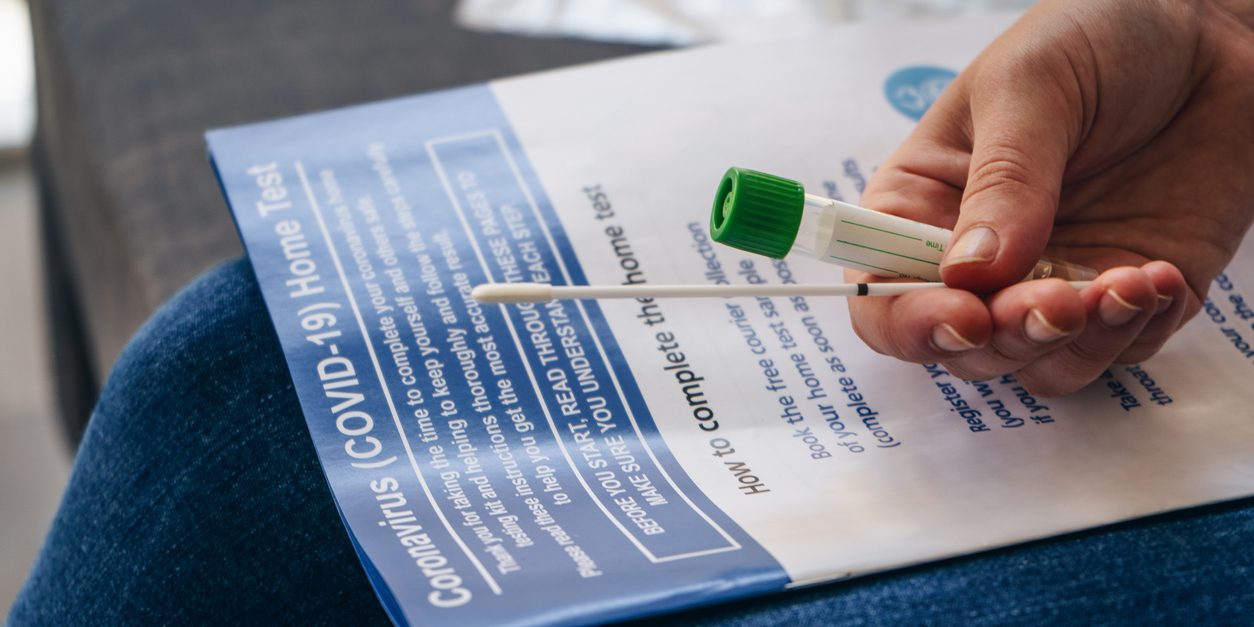
While COVID-19 cases start rising again, more people are once again likely to contract the coronavirus — and that usually involves getting tested. But for employees in your group health plan, they have many options for obtaining a test with no out-of-pocket costs.
Under an executive order issued by President Biden, employees in a group health plan are eligible to receive COVID-19 at-home test kits with no cost-sharing, copay, coinsurance or deductible. Additionally, most health plans are also covering tests performed at hospitals, clinics and pharmacies.
While we told you about these new rules a few months ago, it’s likely that a good many of your employees don’t know about it. With that in mind, you may want to disseminate information to them about how they can be reimbursed by their insurer for COVID-19 tests they purchase.
Here’s what your employees need to know:
Steps for reimbursement
Procedures will vary from insurer to insurer, but the order requires that health insurance carriers reimburse members for up to eight tests a month and no doctor’s order, prior authorization or prescription is required. This applies to any tests they purchased on or after Jan. 15, 2022.
Most health plans have preferred pharmacies that they urge their enrollees to go to for their take-home COVID-19 tests. In these instances, the plans will typically cover the cost at the point of sale so that the health plan member doesn’t have to pay out of pocket.
Covering costs upfront eliminates the need for members to submit reimbursement forms.
However, if they go to a non-network pharmacy or drugstore or purchase a kit online, the health insurer is still required to reimburse them for a test up to $12 (or the cost of the test if it’s less than that).
In these cases, the employee will have to pay for the test upfront and then seek reimbursement from their health insurer.
You can contact your health insurer for information and resources for how your staff can receive reimbursement. Most insurers have published materials to make it easier for your workers to access COVID-19 tests with no cost to them.
Typically, to be reimbursed for at-home test kits, members must submit the reimbursement form and a receipt that shows proof of purchase, which should include the name of the retailer, including the street address, or, if bought online, the website address; date of purchase; UPC code for the at-home test kit; and the cost of the kit.
The order that health plans cover these tests with no out-of-pocket costs for their enrollees will sunset when the federal public health emergency is declared over.
On-site tests
Health plans are also covering the cost of tests that are administered at pharmacies or in hospital settings after either a doctor ordered a test or if the person was exposed to someone who had COVID-19.
Like at-home tests, insurers will cover the costs of these tests regardless of if they are received in-network or from an out-of-network provider or pharmacy.
The types of COVID-19 tests health insurers currently cover are:
- Individual testing with or without symptoms,
- Testing ordered by a health care provider,
- Testing for contact tracing, known or suspected exposure, and
- Testing before or after travel (COVID-19 screening tests for domestic travel are usually covered by most plans, but enrollees should not expect their plan to cover any testing they do abroad).
After the public health emergency ends, however, it’s likely most insurers will stop covering tests obtained out of network.